In the field of oncology, as we got better at understanding the changes that occur in cancers at a molecular level, we have seen a shift towards precision medicine. Biomarkers are central to this change and can be leveraged to provide important insights at every stage of drug development. By advancing our understanding of cancer pathophysiology and tumor profiling, they play a critical role in the discovery and validation of novel targets and therapeutics. Moreover, in both clinical trials and clinical practice, biomarkers are increasingly utilized to guide treatment decisions and predict or monitor treatment response.
Personalized medicine seeks to direct targeted therapies to those patients who are most likely to experience a positive benefit-risk profile while reducing unnecessary exposure to patients who are unlikely to respond. Biomarker-guided trials are essential for enhancing access to targeted therapies, but designing and executing these studies can be a complex endeavor. Thorough planning and a clear understanding of the overarching study objectives are essential for fulfilling the promise of delivering better outcomes to patients in need of life-changing medicines.
In this blog, we review key factors that should be considered during study design to ensure that your biomarker-guided clinical trial can produce meaningful results.
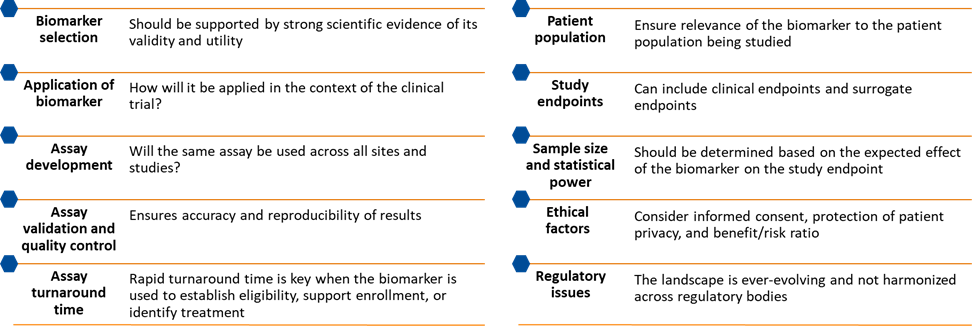
Figure 1. Key considerations for designing biomarker-guided clinical trials
Top 10 considerations for study design in biomarker-guided clinical trials
- Biomarker selection. Biomarker discovery is closely tied to new drug discovery. Biomarkers should ideally be introduced at the start of the drug discovery process at target selection stage. The biomarker chosen should be supported by strong scientific evidence of its validity and utility as a diagnostic, predictive or prognostic marker. It is critical to establish or confirm the clinical relevance of the selected biomarker in the disease of interest. The biomarker should also be feasible to measure and should have good reproducibility across different laboratories and assay platforms to limit variability.
In addition, developing a deep understanding of the prevalence of the biomarker of interest can help sponsors and CROs identify the most promising geographies, sites, and project enrollment rates. - Application of the biomarker. Determine how the biomarker will be applied in the context of the clinical trial. Will it serve as a selection criterion? A stratification element? A response monitoring tool? The intended use of the biomarker data will inform the level of validation required for the biomarker assay in clinical trials.
- Assay development. Select an assay type that is feasible for use not only in a clinical trial, but also in clinical practice. If an assay requires a specialized platform or fresh samples, there may be challenges associated with deployment and logistics. Minimizing variability is key during the assay development process and utilizing a central lab during a clinical trial can ensure consistency in analysis.
- Assay validation and quality control. Biomarker validation or the validation of analytical assays, i.e. precision, accuracy, detection limit and robustness is critical for ensuring that biomarker measurements are accurate and reproducible, both across time and between laboratories. The level of validation required—and the amount of time needed to complete that validation—will depend on how the biomarker is applied. Thus, it is critical manage the validation process such that the assay is ready in time to support the study.
- Assay turnaround time. If the biomarker is to be used to establish eligibility, stratify enrollment, or assign treatment, an assay with a rapid turnaround time is essential for making the biomarker usable in a clinical trial setting. If the biomarker is going to be analyzed retrospectively, managing turnaround time will be less of a priority, but understanding sample storage requirements to ensure assay validity over time will be crucial.
- Patient population. The patient population should be carefully defined based on the biomarker being tested. The biomarker should be relevant to the patient population being studied, and potential participants should be screened and selected based on their biomarker profile.
- Study endpoints. The study endpoints should be carefully selected to reflect the goals of the trial. The endpoints should be relevant to the biomarker being tested and may include both clinical endpoints, such as overall survival, and surrogate endpoints, such as progression-free survival.
- Sample size and statistical power. The sample size should be determined based on the expected effect size of the biomarker on the study endpoint, the expected prevalence of the biomarker in the patient population, and the statistical power required to detect a significant treatment effect. By targeting patients with known mutations, biomarker-guided studies may be able to achieve statistical significance while enrolling fewer patients than traditional trials.
- Ethical factors. The ethical considerations of the trial should be carefully considered, including informed consent, protection of patient privacy, and the balance of study-related risks and benefits. Patient perspectives and regulations on data privacy may vary widely from region to region and these variances need to be factored into the study design.
- Regulatory issues. The backdrop continues to evolve, and requirements for biomarker-guided trials are not harmonized across regulatory bodies. New guidance is being issued on an ongoing basis, so scheduling early meetings—and maintaining an open dialogue—with regulatory agencies during study design mitigates the risk of downstream trial delays.
Increasing the likelihood of approval
An analysis of over 9,700 development programs from 2011 to 2020 found that the use of patient preselection biomarkers increases likelihood of approval.1
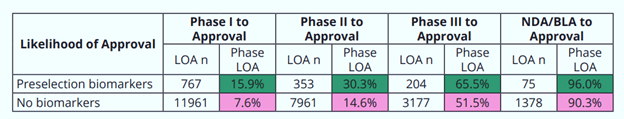
Figure 2. Use of preselection biomarkers increases likelihood of approval at every phase of development1
Clinical trials with biomarker involvement tend to be resource-intensive and may be less efficient due to the level of effort involved in recruiting and enrolling participants. However, with proactive planning, using biomarkers to inform enrollment and treatment decisions can reduce overall study timelines and increase the overall probability of clinical trial success.
To learn more about operationalizing biomarker-guided oncology clinical trials, click here.
[1] BIO. Clinical Development Success Rates and Contributing Factors 2011-2020.
